In the hustle of modern life, waiting for pain to strike before seeking medical attention has become a risky habit. Many people rely on temporary painkillers or massage patches to mask symptoms, while the crucial practice of musculoskeletal screening is overlooked.
Musculoskeletal screening: what it is, what it is not, and what you receive

Musculoskeletal screening is a structured clinical check of your posture, joint function, spinal alignment, and movement patterns to detect early signs of musculoskeletal disorders before they develop into persistent pain. It typically combines history-taking, physical examination, functional movement testing, and—when clinically indicated—diagnostic imaging such as digital X-ray.
This is not the same as treatment. Screening is the decision stage that identifies risk factors, flags potential structural or neurological issues, and clarifies what care is appropriate next, such as self-care, physical therapy, conservative spine care, referral to a medical specialist, or urgent evaluation.
What you receive after a screening (deliverables)
After the appointment, you should expect:
- A clinical summary report with key findings from posture checks, range of motion assessment, orthopedic tests, and neurologic screening.
- A risk level classification (low, moderate, or high risk) based on symptoms, exam findings, and red flags.
- A prioritized next-step plan that explains what to do now, what to avoid, and when follow-up should occur.
- If imaging is done, a documented imaging interpretation reviewed together with clinical findings, including limitations and indications for further tests.
Many spinal and joint issues progress quietly, and screening helps you act on correct information rather than guessing with temporary symptom relief.
This guide explains why you should not delay, the real consequences of negligence, and how a documented screening process can help you make safer decisions for your spinal health.
The real-world consequences of delayed musculoskeletal screening

The musculoskeletal system is the foundation of human movement. When structural misalignments and function limitations are not detected early, the patient may face compounding problems over time.
Missing the “golden window” for recovery
In physical care and rehabilitation, timing matters. In early stages of spinal misalignment, vertebrae may shift slightly and intervertebral discs may not yet be severely compromised. At this phase, conservative care and corrective strategies are often simpler and more time-efficient. However, when the root cause is left unchecked, the condition may progress into chronic degeneration that can be harder to manage and may require longer timelines.
Muscle atrophy and restricted mobility
The spine houses the spinal cord, the pathway of information between your brain and body. Prolonged nerve root compression acts like a bottleneck. When a nerve is irritated or compressed, signals to the muscle can be impaired. Over time, muscles may weaken, and some people notice reduced grip strength, decreased endurance, or difficulty walking.
Escalating financial pressure
Many people assume screening is an unnecessary expense. In reality, preventive care is often an investment that reduces downstream costs. Managing advanced cases—such as severe herniated disc symptoms requiring complex interventions—can be far more expensive than periodic screening. Indirect costs can also add up, including missed work, reduced productivity, and prolonged recovery time.
Severe decline in quality of life
Chronic pain is not only physical but also psychological. Persistent discomfort can lead to sleep disruption, fatigue, and elevated stress levels. This creates a cycle where pain reduces productivity and limits participation in family activities, lowering overall well-being.
What happens during a musculoskeletal screening
A complete musculoskeletal screening typically includes four layers designed to produce repeatable, documented findings.
Clinical history and symptom mapping
Your clinician reviews onset, duration, and aggravating or relieving factors. Symptoms are mapped by location and pattern, including local pain, radiating pain, numbness or tingling, weakness, morning stiffness, and movement-related discomfort. Prior injuries, surgeries, and previous imaging are noted because they influence clinical interpretation.
Posture and movement analysis
Posture assessment looks for visible asymmetries and load patterns, such as head-forward posture, rounded shoulders, pelvic tilt, scoliosis indicators, and uneven weight distribution. Functional movement checks may include squat mechanics, hip hinge, gait observation, and balance screening when relevant.
Range of motion and orthopedic tests
Range of motion (ROM) testing evaluates mobility limits in the cervical spine, thoracic spine, lumbar spine, hips, shoulders, and other relevant joints. Orthopedic tests help differentiate common patterns such as nerve irritation, disc-related pain, joint dysfunction, and soft-tissue involvement.
Neurologic screening
A basic neurologic screen may include muscle strength testing, reflexes, dermatomal sensation checks, and nerve tension tests. This layer is important for identifying cases that require medical referral or urgent evaluation.
Red flags that require urgent medical evaluation

Musculoskeletal screening is not a substitute for emergency care. Seek urgent evaluation if you have any of the following:
- Progressive weakness, foot drop, or loss of coordination
- New bladder or bowel control issues, or saddle numbness
- Severe trauma, suspected fracture, or unexplained severe pain
- Fever, unexplained weight loss, or a history of cancer with new pain
- Severe night pain not relieved by rest, or rapidly worsening symptoms
When imaging may be recommended (and when it may not)
Digital X-ray may be recommended when clinical findings suggest structural changes that affect decision-making, such as a history of trauma, persistent symptoms, suspected instability, visible deformity progression, or neurologic signs that require clarification. Imaging should be interpreted together with the physical exam because X-ray findings do not always match symptom severity.
In many routine cases, especially early or mild symptoms, clinicians may start with physical examination and functional assessment first. The goal is to use imaging when it changes the plan, rather than using it by default.
Common musculoskeletal conditions often overlooked
Many people assume aches and pains are signs of temporary fatigue. However, clinical examination findings may point to underlying structural or functional problems that deserve attention.
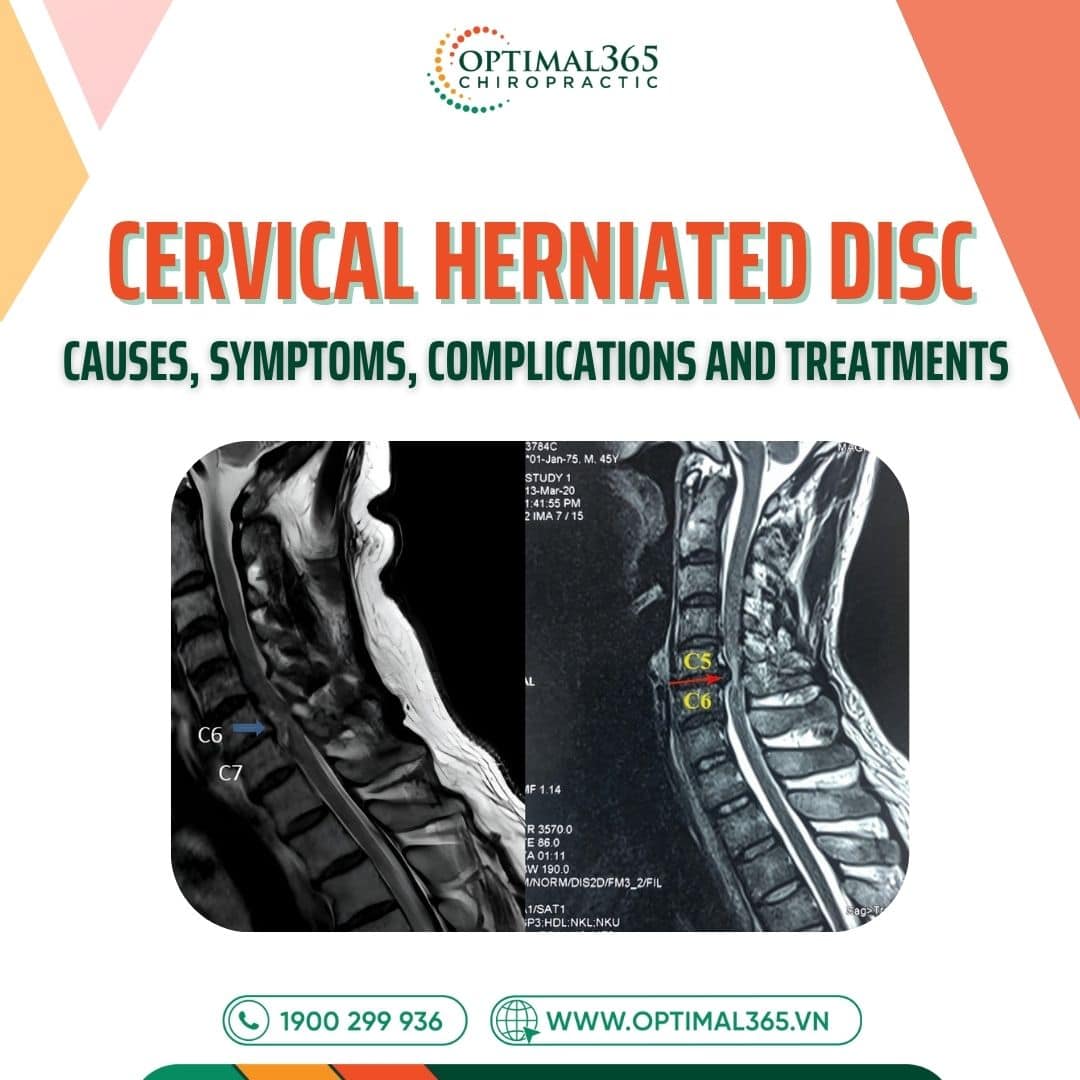
Disc herniation
The intervertebral disc acts as a shock absorber. When the outer layer tears, the inner gel can protrude and irritate nearby nerves. Typical symptoms include numbness, tingling, or a burning sensation radiating from the lower back down the legs, or from the neck into the arms.

Spinal degeneration
Aging is natural, but premature degeneration has become common due to modern lifestyles. Prolonged poor posture accelerates wear and tear over time. Vertebrae may develop bone spurs, discs can dehydrate, and ligaments may thicken, resulting in stiffness and reduced flexibility.
Scoliosis
A healthy spine usually appears straight when viewed from behind. In scoliosis, the spine curves to the left or right and may also rotate. This condition can progress silently. If curvature is not monitored and managed appropriately, it can worsen and contribute to functional limitations.
Neck and shoulder pain patterns
Many people experience neck and shoulder pain linked to posture strain, prolonged computer work, or joint and soft-tissue overload. When symptoms persist, screening helps determine whether the driver is muscular tension, joint restriction, nerve irritation, or movement imbalance.
Benefits of early musculoskeletal screening at Optimal365

At Optimal365 Chiropractic, we recommend screening even when pain is not severe, because many issues develop gradually and remain “silent” for a long time.
Detecting asymmetries and risk patterns early
The body can compensate for misalignments and movement restrictions for years before reaching a breaking point. Early-stage posture changes, movement dysfunction, or developing scoliosis may cause little to no pain at first. A structured exam and appropriate imaging, when indicated, can help identify these risks earlier.
Optimizing with conservative approaches
Optimal365 focuses on non-invasive care that aims to reduce dependence on drugs and avoid unnecessary procedures where possible. Early detection often makes conservative strategies more feasible and may shorten the overall care timeline.
Saving time with clearer decisions
Correcting minor deviations and improving movement habits is often simpler than managing long-standing patterns. Screening provides a documented baseline and helps reduce trial-and-error.
Understanding biomechanics for long-term spinal health
Screening results provide practical information about your posture and spinal mechanics. Your clinician can provide tailored advice on ergonomics, posture habits, and corrective exercises to support long-term improvements.
Groups that need urgent musculoskeletal screening
Based on clinical risk patterns, the following groups should consider screening early.
Office workers
Long hours at a computer, repeated neck flexion, and prolonged sitting increase risk for neck strain, cervical and lumbar overload, and repetitive stress conditions. Screening helps identify posture patterns and movement deficits before symptoms become persistent.
Sports enthusiasts
High-intensity movement increases risk of trauma and muscle imbalances. Screening can identify biomechanical faults that raise injury risk and may also support performance optimization.
Postpartum women
Pregnancy changes the pelvis and spine, and repetitive baby-carrying can overload the lower back and neck. Screening helps clarify which structures are under stress and which corrective steps are appropriate.
Middle-aged adults (over 35)
Discs naturally lose hydration and joints gradually lose flexibility. Signs such as morning stiffness or discomfort during weather changes may indicate early degeneration or mobility limits that benefit from early assessment.
Optimal365 Chiropractic: screening and care process
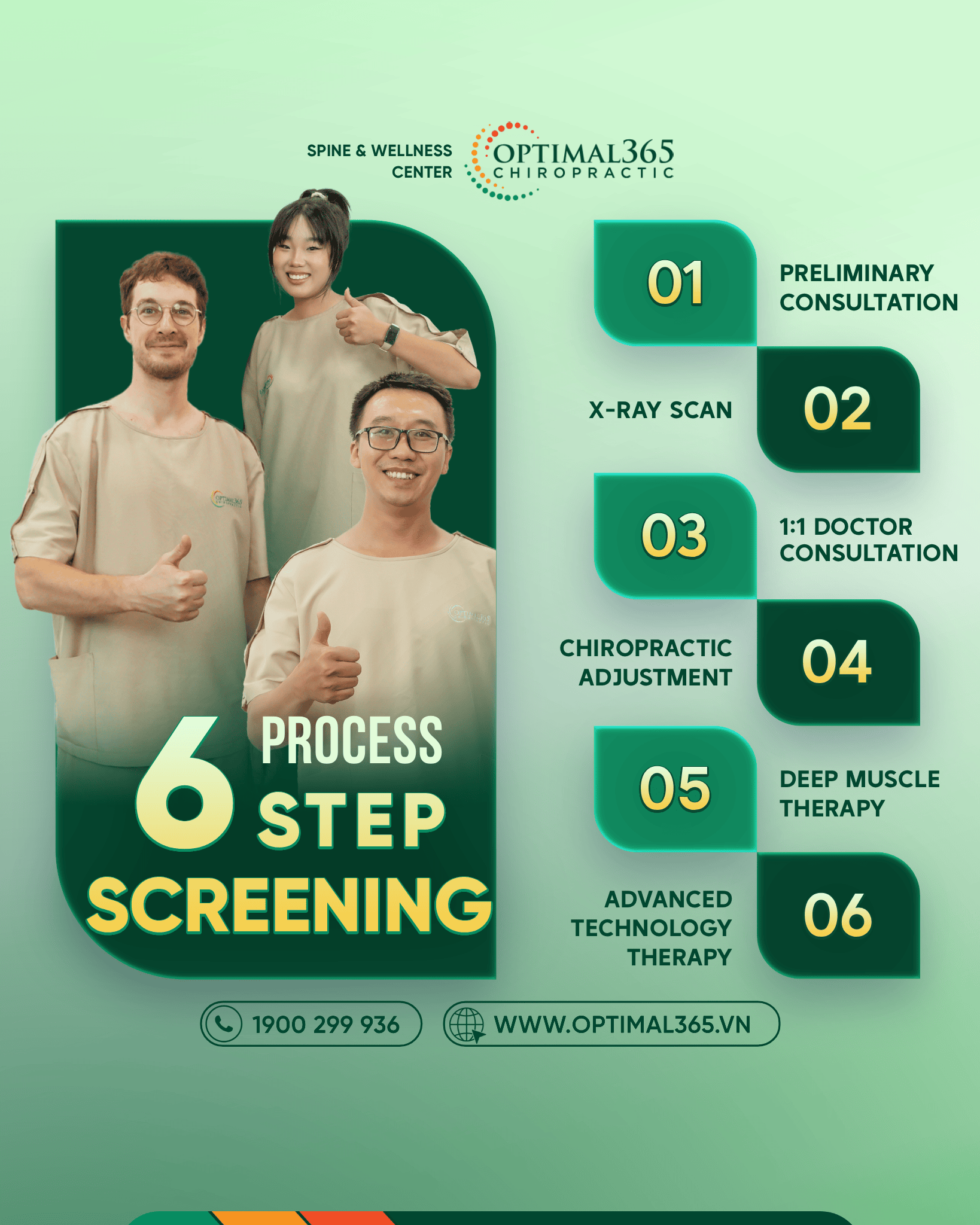
At Optimal365 Chiropractic, the screening process is designed to be repeatable and documented so results can be tracked over time. The goal is to combine clinical exam findings with appropriate tools to support safer decision-making.
Preliminary consultation
Your journey begins with a structured intake that reviews your daily habits, symptom triggers, prior injuries, and any previous imaging. Key tension areas and functional limitations are noted to personalize the examination.
Posture, mobility, and functional assessment
The clinician assesses posture markers, movement patterns, and range of motion baselines. Orthopedic tests may be used to stress specific structures safely, and results are recorded for follow-up comparison.
Neurologic screening
When symptoms suggest possible nerve involvement, basic neurologic checks may include strength testing, reflexes, sensory mapping, and nerve tension tests. Findings help decide whether conservative care is appropriate or whether referral is needed.
X-ray scan (when clinically indicated)
If clinical findings suggest imaging will change the plan, digital X-ray may be recommended. The purpose is to visualize structural alignment and support the clinical picture rather than replacing it.
1:1 Doctor consultation and report review
A doctor reviews your exam findings and any imaging results with you. You receive a clear summary of what was observed, what it may imply, what it does not confirm, and what the next steps should be.
Conservative care options (when appropriate)
If a care plan is recommended, it may include conservative manual techniques to improve joint mobility, soft-tissue approaches to reduce mechanical overload, and targeted corrective exercises. Many clients report improvement, but response varies by condition and chronicity, and progress is monitored using repeatable metrics rather than promises of immediate results.
Advanced technology therapy (when appropriate)
When clinically appropriate, supportive modalities such as shockwave, laser, or ultrasound may be integrated to support soft-tissue recovery and reduce inflammation. These options are selected based on assessment findings and individual needs.
Contraindications and safety notes
Certain situations require modified assessment or referral, such as suspected fracture, severe osteoporosis risk, unstable neurologic symptoms, active infection, or post-surgical red flags. Your clinician should explain what is safe to do today and what requires medical clearance or specialist evaluation.
What happens after the screening results
After screening, the next step depends on your risk level and findings.
Low risk
You may receive posture education, ergonomic adjustments, and a home exercise plan, along with a clear follow-up checkpoint to confirm progress.
Moderate risk
A conservative plan may be recommended, typically combining manual care with corrective exercises and lifestyle adjustments. Goals should be measurable, such as improved range of motion, reduced symptom frequency, and increased functional tolerance.
High risk or red flags
If red flags or significant neurologic signs are present, you may be referred for additional testing, specialist consultation, or urgent evaluation as appropriate.
You should leave with a clear plan for what to do this week, what to avoid, what improvement markers to track, and when reassessment happens.
How progress is monitored
If a care plan is recommended, outcomes can be monitored using objective checkpoints:
- Baseline versus follow-up range of motion changes in the cervical and lumbar spine
- Functional tolerance, such as sitting time, walking distance, or lifting tolerance
- Symptom frequency and triggers, including headaches, radiating pain, or numbness patterns
- Neurologic changes when relevant, including strength, reflexes, and sensory mapping
- Re-assessment schedule with decision rules for escalation or referral
Book your screening today
Musculoskeletal health supports your ability to move, work, and live with confidence. If you want a documented baseline of your posture, mobility, and spinal health, schedule a musculoskeletal screening. You will receive a written summary of findings, a risk level assessment, and a practical next-step plan based on your exam results.
👉 Musculoskeletal screening – Optimal365: Contact us to schedule your appointment!